I'm a physiotherapist, share all my experiences with the patients with all the details about the conditions, also provide easy notes for the student.
Saturday, 31 October 2020
ROLE OF PHYSIOTHERAPY IN ICU
BRRUNSTORM'S APPROACH, EASY AND IMPORTANT NOTES, VERY EASY TO UNDERSTAND
BRUNNSTORM'S APPROACH
INTRODUCTION
It was developed by Signe Brunnstorm, a Swadish American physiotherapist. It is a neurophysiological treatment approach, that has been conceptualised from two important theories of motor control namely- a)Reflex Control Theory b)Herarchial Control theory
a) Reflex Control Theory:- In this theory, reflexes are the building blocks to complex motor control and movement.It says that afferent sensory inputs are necessary prerequisite for efferent motor output. We can understand this by an example:- In acute hemiplegic patients, at day 1 or day 2, there is no movement or flaccidity, there is no reflex activity or no movement. In this situation, brunnstorm states that we should first utilise techniques which will facilitate and use reflex to regain motor control in hemiplegic patients.
b)Hierarchial Control Theory:- It states that CNS is organised in hierarchy levels to control motor functions of the body.
PATHOPHYSIOLOGY
*In normal individual, the motor response of the mid brain, brainstem and spinal cord are controlled by the higher centers (cortex).
*Certain motor behaviours at subconscious and reflexive levels are processed at spinal cord, brainstem and mid-brain level.
*Stroke appears to result in development in reverse, recovery of voluntary movement post stroke proceeds in sequence --
- first the therapist should try to facilitate reflexive movements that are mediated by brainstem and spinal cord.
-followed by more complex movements that are mediated by mid-brain. (flexor synergy, extensor synergy)
-once the patients gain control over these synergies, then brunnstorm recommends now we should progress towards producing more complex motor behaviour which are mediated by higher centers (cortex).
*Proprioceptive and exteroceptive stimulus can be used to evoke desired motor or toner changes
* Progress the patient from lower to higher motor center.
BASIC LIMB SYNERGIES
Limb synergies are intensive of associative reaction. They may occur either reflexively or as early stage of voluntary control when spasticity is present.
When the patient initiates movement at one joint, all the muscles that are linked in synergy with that movement automatically contract causing stereotypyped movement pattern.
Hemiplegic patient cannot perform isolated movements when they are bound by any synergy, example:- a hemiplegic patient wants to flex his elbow, then he won't be able to do it without producing scapular retraction and elevation and shoulder abduction. So everytime he want to flex the elbow, he will be accompanied by activation of rest of muscle of this synergy.
-: UPPER-LIMB SYNERGY:-
-:FLEXOR SYNERGY
-: EXTENSOR SYNERGY
-: MIXED SYNERGY
1. FLEXOR SYNERGY
2. EXTENSOR SYNERGY
3. MIXED SYNERGY
-: LOWER LIMB SYNERGY
-:FLEXION SYNERGY
-:EXTENSOR SYNERGY
-: MIXED SYNERGY
1.FLEXOR SYNERGY
2. EXTENSOR SYNERGY
3. MIXED SYNERGY
Friday, 30 October 2020
Amputation (Causes, level) along with its Physiotherapy management
Defination:-
Removal of limb, partly or totally, from the body, is termed as Amputation. Disarticulation is removing the limb through a joint.
Indication:-
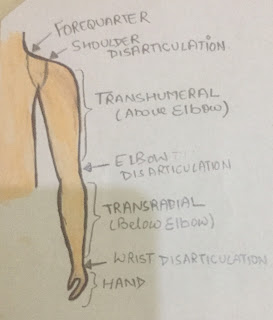
Level of Amputation:-
UPPER EXTREMITY
👉 Forequarter amputation - Also known as scapulothoracic amputation. It is carried out proximal to the shoulder joint. In this type of amputation, part of scapula and clavicle are removed along with the shoulder girdle muscles.
👉 shoulder disarticulation- It is the removing of shoulder joint, but is generally not so popular.
👉 Above- elbow amputation- Also known as Transhumeral amputation. A 20-cm-long stump from the tip of the acromion is measured.
👉 Below-elbow amputaion- Also known as Transradial amputation. The optimum length of the stump is 20cm from the tip of olecranon.
👉Krunkenberg amputation:- In this, the forearm is split between the radius and ulna to provide the pincer grip. The patient can hold a spoon or lighter objects with this 'fork'. 'Hook' prosthesis can be put over this stump for cosmetic purpose.
👉Amputation through the hand:- In this, many forms of amputation are performed through the hand i.e. through metacarpals, etc.
LOWER EXTREMITY
👉 Hindquarter amputation:- Also known as Transpelvic amputation. In this, part of pelvis is removed along with the lower extremity.
👉 Hip disarticulation:- The femur is removed from the acetabulum is performed.
👉 Above knee amputation:- Also known as transfemoral amputation. The optimum length of the stump is about 25-30 cm measured from the tip of the greater trochanter.
👉Knee disarticulation:- It can be performed through the knee as well but not acceptable cosmetically.
👉Below knee amputation:- Also known as transtibial amputation. It is most commomly performed amputation. In this, the optimum length is 14 cm from the tibial tubercle. A patellar tendon bearing (PTB) prosthesis can be fitted over the stump of adequate length.
👉Syme's amputation:- In this operation, the tibia and fibula are divided just above the ankle joint then the skin over the heel is attached back to the stump end of the stump with or without calcaneum.
PHYSIOTHERAPEUTIC MANAGEMENT OF THE AMPUTEE
The management is divided into three stages:-
1. preoperative stage:-
2. Early postoperative stage:-
Management of the stump
3. Mobility stage:-
Frozen Shoulder ( causes, symptoms, stages, physiotherapy management)
WHAT IS FROZEN SHOULDER?
STAGES OF FROZEN SHOULDER:-
👉 Frozen shoulder is self-remitting condition in which the symptoms vanish completely in 18 months of time.
CLINICAL FEATURES OF FROZEN SHOULDER:-
SPECIAL TESTS
SCARF TEST
SHOULDER SHRUG SIGN
APLEY'S SCRATCH TEST
MANAGEMENT OF FROZEN SHOULDER:-
Patient education:- For treatment of frozen shoulder, patient education is very important in helping to reduce frustration and encourage compliance. It is also helpful to create Home Exercise Program which can treat the condition more early.
Physiotherapy management will depend upon the stage--
1. ACUTE PHASE
Relief of pain and spasm is the main focus of this stage, which is controlled by application of ice pack, ice massage, TENS.
During this stage, any activity that can cause pain should be avoided. Better results have been found in patients who performed simple pain free exercises, rather than intensive physical therapy.
A pulley may be used to assist range of motion, depending on patient's ability to tolerate the exercise.
Isometric strengthening of rotator cuff muscles, pendulum exercises are performed .
2. SUBACUTE PHASE
U.S is given to break the adhesion in capsule which is given into posteroinferior area.
Gentle and specific shoulder joint mobilisation and stretches are performed to regain range and strength of the joint.
Mobilisation with movement (MWM) appears to be most effective and more effective than stretching exercises alone.
Care must be taken not to introduce exercises that are too aggresive.
👉 capsular stretches are performed (anterior , posterior and inferior stretches)
3. CHRONIC PHASE
Strengthening exercise are also included along with the progression of all the above exercises.
The stretch can be held for longer duration and sessions per day can also be increased.
Pulley and WAND exercises are also introduced in the treatment programme.
Home Exercise Program is given to the patient to reduce the chances of relapsing of the condition.
Tuesday, 27 October 2020
MCKENZIE METHOD
INTRODUCTION
McKenzie method is a technique used in physical therapy. It was developed by Robin Mckenzie, a New Zealand. This is also known as Mechanical diagnosis and therapy(MDT). It is a system comprising of assessment, diagnosis and treatment for the spine and extremities.
In this, the physiotherapist finds out the relationship between causes, effects and the positions of the patients he assumes while sitting, standing or moving, and the location of pain as the result of these positions or activities.
So this approach requires the patient to move through a series of activities and tests movements to elicit the patient's pain response. Then therapist uses these information to develop an exercise program to reduce the pain.
AIMS
👉 Reducing pain
👉 Centralisation of symptoms
👉 Complete recovery of pain
STEPS
1. ASSESSMENT:- In this step, the therapist takes the history of the patient, checking the pain aggrevating and relieving positions and also rules out the RED FLAG SIGNS.
*RED FLAG SIGNS like anorexia, weight loss history, presence of night pain and ON/OFF fever.
2. TREATMENT:- This is based on assessment and it varies from person to person. The therapist teaches the patient that positions which can relieve his pain.
3. PREVENTION:- This step is done to minimize the reoccurence of the conditions. It tells the patients about the factors and causes that will aggrevate the pain.
MCKENZIE CLASSIFICATION
👉 POSTURAL SYNDROME:- This is basically due to attaining the wrong posture for longer period of time. Pain subsides after changing the posture. It is common in younger age group(below 30 years). The cause is the overstretching of the normal tissues because of poor sitting or standing postures or lack of stretching exercises in sedentary professions.
👉 DYSFUNCTION SYNDROME:- This is caused by mechanical deformation of soft tissues affected by adaptive shortening. Pain is produced as shortened structure are stressed by end range.
👉 DERANGEMENT SYNDROME:- In this, anatomical disruption or displacement occurs within the intervertebral disc. In younger age group, there is displacement of the annulus complex or fluid nucleus, whereas in older age group degenerated annulus or fibrosed nucleus may be present.
DIRECTIONAL PREFERENCE
It describes the situation when movements in one direction will improve pain and limitation of range, whereas movements in opposite direction cause sign and symptoms to worsen.
👉 CENTRALISATION:- In this, limb pain emerging from the spine is progressively abolished in a distal to proximal direction in response to treatment.
👉 PERIPHERILIZATION:- Pain emerging from spine spreads distally into the limb by the treatment. If this occurs, the treatment strategy should be avoided.
Monday, 26 October 2020
Female Athlete Triad
INTRODUCTION
The female athlete triad is a medical condition observed in physically active females. There are 3 components in FAT:-
💧Osteoporosis
💧 Amenorrhea
💧 Eating disorder
It is important to note that all the components of the triad are NOT needed to triad to be present.
Timely prevention, recognition and treatment can delay the progression.
In this diagram, red triangle shows the triad conditions and green triangle shows normal parameters.
1. OSTEOPOROSIS
It is a major health problem. It can be defined as low BMD (Bone Mass Density). This lead to bone fragility and recurrent bone fractures.
CAUSES:- 1. Reduced Ca²+ absorption from intestine
↓
Parathyroid gland activated
↓
Parathyroid hormone is released
↓
increases resorption of calcium from the bones
↓
decreased BMD
2nd reason can be Postmenopausal oestrogen deficiency ( which will lead to decreased calcium absorption)
COMPLICATIONS:- frequent fracture (most commonly hip and wrist)
:- fall risk increases
2. AMENORRHEA
Menstrual function ranges from enumenorrhea (menstrual cycle 28 +7/-7 days) to amenorrhea ( absence of menstrual cycle for >90 days). It may be primary ( 1st menustral cycle is delayed) and secondary ( when menstral cycle has begun).
CAUSES:- It can be due to weight loss, stress, excessive or wrong exercises.
3. EATING DISORDERS
There has been a relationship between eating disorder and athletic activity. There are some sports in which the emphasis on thinness and reduction in body fat like gymnastics, ballet dancing, etc. Pressure from coaches, parents or competitors regarding body shape may lead to abnormal eating pattern. Other psychological risk factors like low self esteem, anxiety and OCD.
Eating disorder can be: i) restrictive eating pattern ii) classic eating disorder like anorexia nervosa (fear of being overweight) and bulimia nervosa (binging followed by avoid weight gain.
SYMPTOMS OF FAT
Absent or abnormal periods, acne, bone loss, excessive facial hair, fatigue, hair loss, headache, pelvic pain, vision changes, weight loss.
TREATMENT OF FAT
Female athlete triad is a serious disorder and requires treatment. The main goal of the treatment is to normalise the menstrual cycles and to improve bone density.
Diet and Exercises:
The doctor would discuss the patient’s eating habits and suggest changes to improve nutrition in order to meet body requirements. The patient exercise routine is also revised to maintain healthy body weight.
Medications:
- The doctor would prescribe hormonal therapy to treat amenorrhea. Usually oestrogen and progesterone are prescribed to treat the altered menstrual periods. These hormonal medications also help to improve bone health.
- After evaluating the patient, the doctor would prescribe calcium and vitamin-D supplements to prevent bone weakness.
- However, the patient requires support from doctor, coaches and other family members for successful treatment of this condition.
Psychological Management:
It is one of the most important yet underutilized management strategies for this condition Patients with female athlete triad are often very competitive people and changing their mentality is not very easy. Psychological counselling is required for managing patient behavior. Mental health intervention is more important in patients with established eating disorders such as anorexia nervosa or bulimia nervosa.
IMPINGEMENT SYNDROME
INTRODUCTION:- Impingement is the inflammation produced by the injury of rotator cuff muscles around coracoacromial arch. It occurs mostly in throwers and patient comes with the chief complaints of having difficulty in performing overhead rotational movement.
CAUSE:- The cause of impingement can be -
i) supraspinatus tendonitis
ii) bicipital tendonitis
iii) coracoacromial bursitis
iv) calcification in any of above tendons leading to tear.
v) hook type of acromion.
CLINICAL FEATURES:- The patient generally fall in the age of 40-60 years. ROM of forward flextion and abduction is restricted beyond 100 degree in internally rotated position. Effusion may or may not be present. Instability may or may not be present.
SPECIAL TESTS:-
-: PAINFUL ARC TEST:-
Purpose of Test- To test for the presence of subacromial impingement.
Test Position- Sitting or Standing
Performing the Test- In this, the patient is asked to elevate (either flexion or abduction) the arm. The test is considered POSITIVE if the patient has pain in between 60-120 degrees of the movement.
-: HAWKIN'S KENNEDY TEST:-
Purpose of the Test- For the presence of any impingement of the rotator cuff muscles
Test Position- Sitting or Standing
Performing the Test- The examiner places the patient's arm shoulder in 90 degrees of shoulder flexion with the elbow flexed to 90 degrees and then internally rotates the arm. The test is considered POSITIVE if the patient feels pain with internal rotation.
*To rule out the supraspinatus tendonitis cause of the impingement syndrome. We use EMPTY CAN TEST.
In this, the patient is supposed to perform abduction in scapular plane with the thumb pointed downward. Such patient will have pain in the initial range of this movement.
*The location of pain will also vary with both the above cases. In supraspinatus tendonitis, the patient will complain of pain above the spine of scapula upto the acromion.
Sunday, 25 October 2020
Thoracic Outlet Syndrome (Diagnostic tests with its management)
i) brachial plexus
ii) subclavian artery at the outlet of thoracic cage.
CAUSES:- 💧 Tight Scalene muscle
💧 can be associated with dislocation of clavicle.
💧 tight pectoralis minor muscle
💧 presence of cervical rib (extra rib)
💧 adaptive shortening of fascia.
💧 faulty posture
Friday, 23 October 2020
PAINFUL ARC TEST
-: PAINFUL ARC TEST:-
Purpose of Test- To test for the presence of subacromial impingement.
Test Position- Sitting or Standing
Performing the Test- In this, the patient is asked to elevate (either flexion or abduction) the arm. The test is considered POSITIVE if the patient has pain in between 60-120 degrees of the movement.
Thursday, 22 October 2020
Role of Physiotherapy in Rehabilitation
The aim of rehabilitation is "to take the patient from the bed to the job." To achieve this, a large team-organisation is necessary and as a member of this team physiotherapist plays a very important role. The requirements of the physiotherapist or any other member of the team to achieve the great result are:-
👉 the ability to carry out instructions accurately.
👉 the ability and desire to cooperate with the other members of the team, especially with occupational therapist.
👉 observe accurately for evaluation and in the planning for the disabled.
👉 ability to give the patient confidence.
Physiotherapists play a role in:-
💧 PREVENTION
💧 TREATMENT
💧 RESTORATIVE
1. PREVENTIVE ROLE
Assess the physical health and identifying any musculoskeletal, neurological problems that could be aggravated by any means.
To carry out awareness programme in various communities, regions by conducting camps, audio-video tapes, banners with the help of local people or the local resource providers.
To identify the higher risk population and to plan a strategy to overcome that problem.
To arrange meaningful workshops on small scale in different regions or communities to make people aware about general health, hygiene, use of services provided by government.
To plan workshops, focusing mainly on the old age population in the region making the family members aware about the problems that could be face by affected persons. Example: high risk of fall, etc.
To plan workshops to check the risk on pediatric problems in a region.
To prevent any secondary complication of the bedridden patient or patient who are admitted in ICU and cannot move like bedsores, retention of lung secretion, oedema, muscular atrophy.
2. TREATMENT ROLE
Physiotherapist advises some exercises to the patient to achieve therapeutic benefit and these exercises are called Therapeutic Exercises.
Coordination exercises- any patient who is not able to do a purposeful movement due to lack of coordination.
Balance training- balance can be improved by Frankel Exercises
Management of spasticity- by passive stretching of agonist and strengthening of antagonist. Splints and positioning are also done.
Relaxation exercises- deep breathing, etc
Reeducation of muscles with the help of electrotherapeutic modalities like faradic current.
Strengthening exercises- by applying resistance in gradual manner.
Treatment of scars and adhesions.
To treat the pain by different electrical modalities like TENS, U.S., IFT, etc.
3. RESTORATIVE ROLE
In this phase, occupational therapist plays an important role.
Help in getting the individual independent in doing his ADLs.
Make him master of some activities so he can earn for himself.
Help him in gaining self-confidence.
Help him to get out of any depression or low self esteem.
Teach the patient to avoid such factors which can relapse the conditions
Gait training- to make the patient independent
Monday, 19 October 2020
SYRINGOMYELIA
INTRODUCTION
Syringomyelia is a term derived from Greek word. 'Syrinx' means tube or cavity and 'myelos' means spinal cord. Hence it is characterised by elongated cavities lining close to the central canal surrounded by glia. These are often extended upwards to the medulla leading to syringobulbia.
ETIOLOGY
1. CONGENITAL:- In this, there is malformation of the cerebellum which protrude out from its original position to the cervical or neck portion of the spinal cord.
2. ACQUIRED:- Due to trauma, meningitis, hemorrhage, tumour. Here the cyst is formed in spinal cord by one of these cause.
PATHOLOGY
CSF serves to cushion the brain. Excessive CSF in the central canal of the spinal cord dissects into the surrounding white matter and form a cystic cavity or syrinx.
The usual age of onset is 25-40 years but it may be as early as 10 years and as late as 60 years.
SIGN AND SYMPTOMS
Most characteristic symptoms are Anaesthetia i.e. loss of sensation of pain and temperature, but not of touch, vibration or motor. This is due to uninvolvement of posterior column until late.
Muscular atrophy and paralysis occurs as soon as anterior horn cells are subjective to pressure.
The patient usually notices slow onset of wasting and weakness of one hand which may be progress upward upto the trunk.
Feet are also involved but later.
DTR(deep tendon reflexes) are diminished or lost.
Analgesia and thermoanaesthetia have segmental distribution involving 1st ulner side, then radial side and then neck and chest.
Occular paralysis leading to ptosis and smaller pupil.
In severe or chronic cases, ataxia or spastic paraplegia is also seen.
SYRINGOBULBIA
👉 Involvement of medulla also
👉 nystagmus present
👉 vertigo present
👉 motor function of cranial nerve may also be seen.
TREATMENT
Surgery is the treatment of syringomyelia. Physiotherapy treatment is same as we do for a spinal cord injury patient. We will improve muscle power, patient education, frankel exercises for balance, prevt secondary complications, etc.
Saturday, 17 October 2020
TRIGEMINAL NEURALGIA | PHYSIOTHERAPY MANAGEMENT IN TRIGEMINAL NEURALGIA
INTRODUCTION
It is a facial pain syndrome which is characterised by short term, unilateral facial pain following the sensory distribution of cranial nerve V, the Trigeminal nerve. Most commonly, the pain radiates to the mandibular or maxillary regions.
CLINICAL ANATOMY
The trigeminal nerve, the 5th cranial nerve, is the nerve responsible for sensation in the face, and control of motor functions such as biting and chewing. It has three branches:-
i) Opthalmic nerve (V1) - It is sensory nerve receive sensation from the forehead.
ii) Maxillay nerve (V2) - It is again sensory which takes sensation from the maxillary region.
iii) Mandibular (V3) - It is sensory and motor both, controlling the muscles of mastication: Temporalis and Masseter.
MECHANISM OF INJURY
The symptoms of pain is usually caused by compression of the Trigeminal nerve route in CNS. The common cause of compression can be tumor or their associated blood vessels. It can be due to the complication of Multiple Sclerosis and neurological conditions, due to demyelination of the root entry of Trigeminal nerve in the pons.
CLINICAL FEATURES
The pain can come in sharp spasms that feel like electric shocks. Pin generally occurs on one side of the face and may be brought on by sound or touch. Pain can be triggered by brushing teeth, shaving, putting on makeup, touching face, eating or drinking, speaking, etc. 60% of patients with TN present with lacinating pain shooting from the corner of the mouth to the angle of jaw.
DIAGNOSIS
There is no need for any particular diagnosis, as the patient with characteristic history and normal neurological examination may conclude the disease. MRI scanning is often indicated simply to exclude the other causes of the pain, such as Acoustic Neuroma.
DIFFERENTIAL DIAGNOSIS
✔ Atypical facial pain
✔ migraine
✔ Cluster headache
MANAGEMENT
Antiepileptic drugs are very useful in management of TN. Some patient require surgery if condition worsens over time and drug management becomes less effective. Microvascular decompression and radiofrequency thermorhizotomy are the surgical procedure.
PHYSIOTHERAPY MANAGEMENT
The main goal of physiotherapy are:-
✔ to relieve symptoms
✔ to restore functions
✔ to reduce the pain in face and other affected areas
Patient were treated with continues TENS for 20 minutes over the path of the affected nerves for 5 days a week for 4 weeks. One electrode was placed just before the ear, the other one at end of the respective nerve.
To reduce muscle spasm, a hot moist pack was applied on neck and trapezius muscle for 10 minutes, Isometric exercises for each side and pain free neck range of motion exercises (neck flexion, extension, side-flexion) for five repetitions each are given.
Relaxation exercises which includes deep breathing exercises should be performed for 10 minutes.
Distraction techniques are also incorporated, patient are asked to involve in those activities in which they like to perform instead of sitting and thinking of the pain situations.
To reduce hypersensitivity, patient were asked to cover the affected side of their face with the soft cloth or with the cotton pad for 15 minutes per day, which may help in promoting a reduction of the nervous system to constant afferent input.
Finally, the patient is asked to avoid use of cold water for drinking and washing their face, use of a scarf to avoid the exposure of the face to the cold environment and to avoid eating hard food and chewing food on the non-affected side.
Sunday, 4 October 2020
PARKINSON'S DISEASE ( SYMPTOMS, ASSESSMENT, CAUSES,) PARKINSON-PLUS SYNDROME
INRODUCTION:- It is a progressive disorder of the CNS with both motor and non-motor symptoms. The onset is gradual, basically after 50 years. The cause is disturbance in the Dopamine system in basal ganglia. A dopamine deficiency can be due to a drop in the amount of dopamine made by the body or due to reduction of receptors in the brain.
SYMPTOMS:- MOTOR SYMPTOMS include the cardinal features of rigidity, bradykinesia, tremors, and, in later stages postural instability, muscle weakness, festinating gait, etc.
NON-MOTOR SYMPTOMS include sensory symptoms, dysphagia, speech disorder, cognitive dysfunction, depression and anxiety, autonomic dysfunction, sleep disorders.
ASSESSMENT:-
COGNITION:- It examines the memory, orientation, conceptual reasoning, problem solving, judgement. A brief screen of cognitive function can be obtained using MMSE (Mini-Mental Status Examination).
PSYCHOLOGICAL FUNCTION:- It determines the level of depression, stress anxiety, insomnia, anorexia, sadness. All these symptoms should be asked to the patient. Instruments like- Geriatric Depression Scale and Beck Depression Inventory.
VISUAL FUNCTION:- It determines acuity, light and dark adaptation, and accomodation. Patient will experience blurring of vision and difficulty in reading which is not improved by corrective lens.
MOTOR FUNCTION:- A) RIGIDITY- Initially there is asymmetrical rigidity which affects shoulder and neck later affects trunk and extremities. In this, there is determination of type of rigidity whether the rigidity is sustained( lead pipe) or intermittent (cogwheel).
B) BRADYKINESIA- Initially movements are slow, and in later stages, movement become arrhythmic with frequent start hesitation and arrests(akinesia). A stopwatch can be used to count the movement time and reaction time (elapsed time between the patients desire to move and the actual movement response). Timed tests for Rapid Alternating Movements (RAM) can be used to determine the effects of bradykinesia.
C) TREMORS- The location, persistence and severity of tremors should be recorded. Upper limb functional skills such as drinking from a cup, feeding, dressing and writing can be used to test for the effects of tremors.
D) POSTURAL CONTROL- The therapist first observe the patients resting posture in sitting and standing which further changes with movement.
E) BALANCE- Berg Balance Scale (BBS) - Functional Reach Test (FRT) -Timed Up and Go Test (TUG) -Cognitive Timed Up and Go (CTUG) -Dynamic Gait Index (DGI)
F) GAIT- Assess all parameters and characteristics of gait during walking on level surface include start time or gait initiation, speed of walking, stride length, etc. - 6-minute walking test
CARDIOPULMONARY FUNCTION- In this, pulmonary function test, breathing pattern, chest wall mobility and thoracic expansion are checked. Along with these, vital signs like B.P., Respiratory rate, etc are also assessed. 6- or 12- minute walk test can be used to determine endurance capacity. Treadmill, cycle ergometer (arm or leg) are also used.
DISEASE SPECIFIC MEASURES- Parkinson's Disease Questionnaire (PDQ-39) is a 39-item questionnaire. It focuses on eight health-related quality-of-life dimensions (mobility,ADLs, emotional well-being, stigma, social support, cognition, communication and bodily discomfort).
Reflexes and Its Assessment (Deep and Superficial Reflexes)
INTRODUCTION:- Reflexes are the involuntary and instantaneous movement in response of a stimulus. It is an automatic response to a stimulu...

-
INTRODUCTION Concave-Convex rule was given by Freddy Kaltenborn. It is ba...
-
FRACTURE HEALING FRACTURE:- A fracture is a break in the continuity of a bone. The healing of ...
-
BRUNNSTORM'S APPROACH INTRODUCTION It was developed by Signe Brunnstorm, a Swadish American physiother...